Knowledge Translation & Coordination of Practices
Authors: Giulia Di Rienzo (UANTWERP), Prof. Erik Myin (UANTWERP), Dr. Ludger van Dijk (UANTWERP)
The following REPAIRS toolbox is available under the CC-BY licence (Creative Commons: https://creativecommons.org/). This implies that others are free to share and adapt our works under the condition that appropriate credit to the original contribution (provide the name of the REPAIRS consortium and the name the authors of the toolbox when available, and a link to the original material) is given and indicate if changes were made to the original work.
KNOWLEDGE TRANSLATION AND COORDINATION OF PRACTICES
THE KTA GAP
It is frequently stated that the enormous amount of resources being put into biomedical research, and the developments in understanding disease mechanisms, are not resulting in proportionate improvements in new treatments, diagnostics, and prevention. Moreover, there is a considerable delay between the production of research evidence to improve health and well-being and its application into policy and practice. In the clinical sector, this time lag is estimated to be around 17 years.
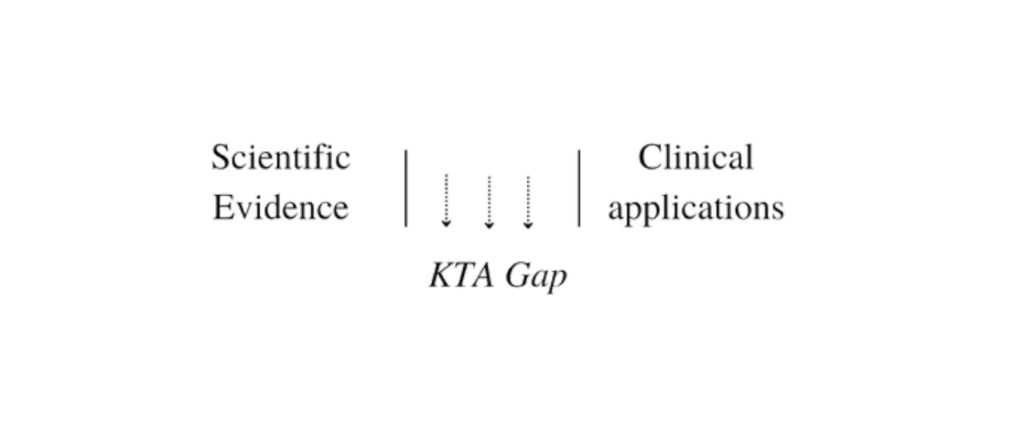
The difficulties have been conceptualized as a “knowledge-to-action” (KTA) gap between scientific results and practical applications.
KNOWLEDGE TRANSLATION
Knowledge translation is a common spectrum of strategies to think about ways to bridge this gap. Knowledge translation (KT) has been defined first in 2000 by the Canadian Institutes of Health Research (CIHR) and then, at a consensus meeting of the World Health Organization in 2005, as «the synthesis, exchange, and application of knowledge by relevant stakeholders to accelerate the benefits of global and local innovation in strengthening health systems and advancing people’s health»[1] .
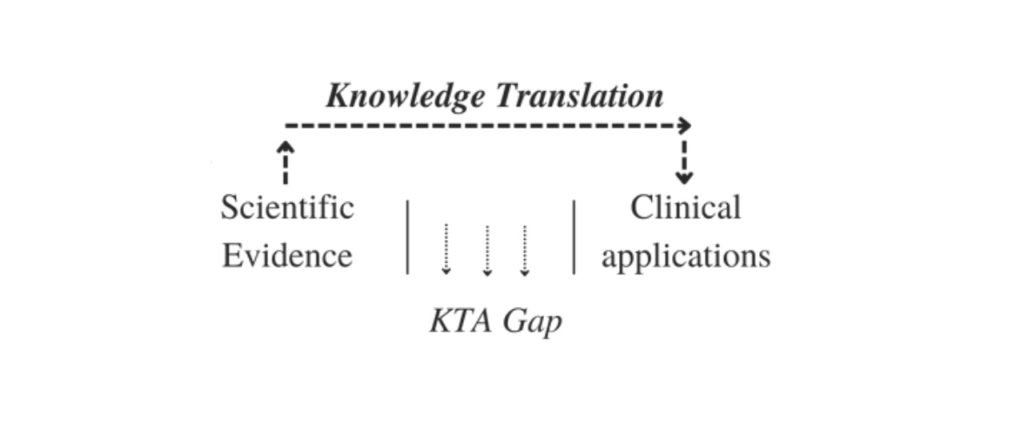
Knowledge translation is then the process of taking research from the laboratory, research journals, and academic conferences, and making it available to people and organizations who can use it for practical purposes.
KT EFFECTIVENESS
There is a large and ongoing debate on the effectiveness of knowledge translation models (Sudsawad, 2007; Bero et al, 1998; Grimshaw et al. 2001), but it is generally underlined that the benefits are modest. Models that normally use interventions that actively address specific barriers to change are said to be more effective, but hardly generalizable. In addition, it is difficult to distinguish which elements of such interventions have led to success. For this reason, the literature concludes that one of the problems to be solved is that there is not enough evidence to support decisions about which knowledge translation strategy is likely to be effective under different circumstances (Sudsawad, 2007).
A SHARED ATTITUDE
The relevant literature on knowledge translation is often so varied that it is difficult to identify a coherent and explicit position (Graham et al, 2006). Undoubtedly contributing to the confusion in the area is the use of multiple terms, which belong to different conceptual backgrounds, to describe all or part of the process. For example, Ian Graham and his colleagues (2008) identified 29 terms used to refer to some aspects of the concept of knowledge to action: «Some of the more common terms applied to the KTA process are knowledge translation, knowledge transfer, knowledge exchange, research utilization, implementation, dissemination, and diffusion» (Graham et al., 2008).
Although there are many ways to discuss knowledge translation[2] they all seem to follow a shared attitude. With ‘shared attitude’, it is not meant something coherent and monolithic as an explicit framework, but rather a tendency to organize solutions. In fact, most researchers focus on developing knowledge infrastructures or knowledge management models to bring new scientific evidence to the clinical world. This is because most of them are based on the same way of understanding the problem, which is that the issue to be solved is a gap between knowledge and its application.
UNQUESTIONED ASSUMPTIONS
According to several authors, this perspective rests on some unquestioned assumptions (see Seely Brown J., Duguid P., 2001; Greenhalgh, T., & Russell, J. 2009; Cook, S. D. N. & Brown, J., 1999):
- Firstly, that the generation of knowledge is cleanly detached from practice, with theory and practice being two temporally distinct phases. Knowledge is considered as a product of scientific practice that, once produced, can be detached from the scientists who generate it and the practitioners who may use it.
- secondly, because the empirical results of the scientific process and the process itself are detached, knowledge is treated as an object that can be handled, reproduced, stored, and transferred largely independently from the communities that produce or possess it. As knowledge-as-object becomes more important, the practical processes from which it came are backgrounded.
A POSSIBLE DIRECTION
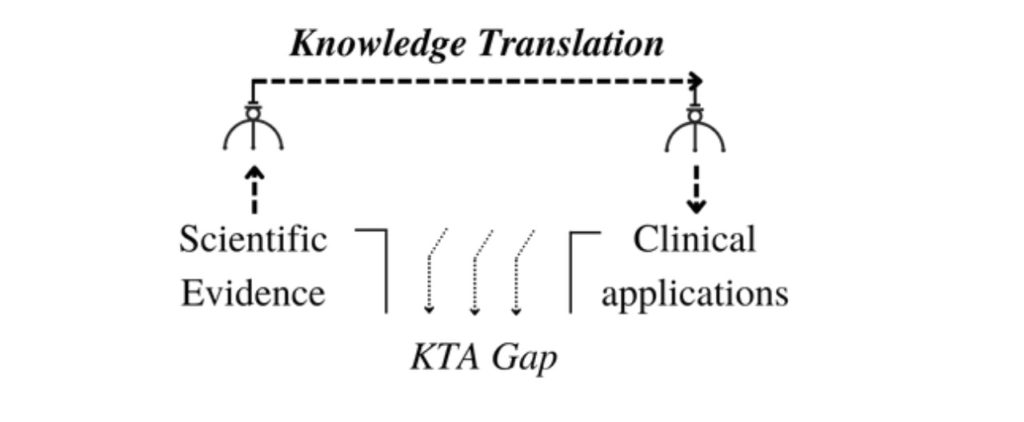
If we follow this line of reasoning, it means we are constraining the strategies of knowledge translation into a sort of “claw-machine” metaphor. The input is a scientific result, which is produced by basic science, while the output is the practical use of this evidence in the clinical setting. Translation research – in this frame – is understood as a claw, leading empirical evidence from its site of origin to application in clinical organizations.
RE-LOOKING AT THE PROBLEM: ITS HISTORY
However, the “knowledge-to-action” gap is a relatively recent problem. Back in the 50s and 60s, basic and clinical research were inextricably linked, as – practically – medical research was mostly done by physicians, i.e., scientists who also treated patients. In the 70s, with the increased popularity of molecular biology, clinical and basic research started to separate and differentiate into several disciplines, with their own training and career paths (Butler, 2008). This separation created several communities, each pursuing different goals, led by different norms and concerns (Restifo & Phelan, 2011), which contributed to making any interchange between them problematic.
CULTURAL, SOCIAL AND MATERIAL DIFFICULTIES
In fact, scientists and clinicians undergo many years of specialized education and apprenticeship-like training, in which students learn to adjust to the research and training field in which they are involved. In the social and material practices they both have been exposed to, in which they actively participated, they have learned dialects, idioms, technicalities, acronyms, different ways of speaking which bind the group they belong to, but which are unintelligible to outsiders. As a result, each group has trouble following the other’s conversations. Moreover, scientists and clinicians do not have a shared value system, even regarding what constitutes knowledge and ignorance. Finally, their “ends-in-view” are shaped by different practical judgments. (Restifo, Phelan, 2011)
THE IMPORTANCE OF CONTEXT AND SOCIO-CULTURAL NORMS
Even in the literature on innovation, understood as the implementation of knowledge, the importance of contextual and inter-relational factors is widely agreed upon. For example, social influences such as the leadership style (Bledow et al., 2009; Tierney, 2008; Chaman et al, 2021), the team environment, participation, constructive controversy, and intra-group safety are said to be fundamental to innovation (Yakhlef & Rietveld, 2019). But emotions and mood seem to play a decisive role. too. Several studies suggested a link between positive mood states and innovation (Aslan & Atesoglu, 2021; Brimhall & Mor Barak, 2018; Yakhlef & Rietveld, 2019; Amabile et al., 2005; Bledow et al., 2009). Interestingly, material and physical aspects are relevant, too, including the working space. For instance, it seems that long corridors facilitate a hierarchical organization, with people working in separate offices, while a flat space allows people to interact regardless of their position and rank (Kristensen, 2004). These findings attribute to sociocultural norms and physical context a significant impact on the way we generate and apply knowledge, and that needs to be taken seriously.
REFRAMING THE PROBLEM
Considering the elements just seen, the problem between basic science and clinical practice expands to issues other than just the transfer of knowledge, it is indeed much deeper as it has to do with the way the communities are used to practice while dealing with very different local situations. In order to find new solutions, it would be helpful to reframe the way we think about the problem and see the problem of knowledge transfer in a broader context.
A typical example to explain what is meant with “reframing” is the “elevator problem”. Imagine the occupants of an office building complaining to the building owner, saying the elevator is too slow. The residents have already framed the problem and decided what needs to be done. Their framing in fact points towards solutions that make the elevator faster, such as upgrading the motor or installing a new elevator. But the problem could also be reframed as “the wait is annoying”, and that issue could be solved by installing other features, such as mirrors, music, etc.
A PROPOSAL: EMBRACING THE PRACTICES
Reframing the problem means focusing on the actual settings and considering the material, social and cognitive aspects and differences of the practices. A possible reframing of the problem could be that there is a discontinuity in the way communities engage with their local contexts and in what is considered relevant for their daily activities. It is still a problem of coordination, not between knowledge and action, but between activities and practices. What becomes important in this reframing, if we think about possible solutions, is to understand how we cooperate and reconfigure our practices. Knowledge translation could then involve reconfiguring practices and experience. Learning to participate in several different doings and changing their criteria for success together, as these practices get coordinated over time.
[1] Note that there are many definitions.
[2] (see for example “Understanding-User-Context Framework” (Jacobson et al., 2003); “The Ottawa Model of Research Use” (Logan and Graham, 1998); “The Knowledge-to-Action Process Framework” (Graham et al. 2006); “The Promoting Action on Research Implementation in Health Services Framework” (Kitson, Harvey, & McCormack, 1998; Rycroft-Malone, 2004; Rycroft-Malone et al., 2002)