Rehabilitation in sport injuries from a systems perspective
Authors: Anaëlle Cheillan (UL), Giacomo Bressanello (UMCG)
The following REPAIRS toolbox is available under the CC-BY licence (Creative- Commons: https://creativecommons.org/). This implies that others are free to share and adapt our works under the condition that appropriate credit to the original contribution (provide the name of the REPAIRS consortium and the name the authors of the toolbox when available, and a link to the original material) is given and indicate if changes were made to the original work.
Introduction:
A paradigm shift in rehabilitation? Defining the conceptual framework
One can address this broad topic with a fundamental question: ‘What is rehabilitation?’. Borrowed from the Latine habilitāre (“to give ability to”), itself derived from habilis (“skilled”, “handy”) and habeo (“have in hand”), the term “rehabilitation” can be defined as the process of giving back the ability to control motor skills to patients with motor disorders. Teaching a new (or previously lost) motor skill and assessing the outcomes of (re-)learning processes thus are important tasks for therapists in various clinical settings. While these professionals all share the common goal of improving a patient’s activities in daily life, their approaches towards this goal can be based on different, conflicting, theories of motor learning. Conceptual divergences in motor learning should not, however, be overlooked, as they can lead to fundamentally different interpretations of the movement outcomes or disorders observed in patients. These differences extend to the application of diverse assessment and training methodologies, each of which uniquely influences the learner’s practical abilities (1,2). Furthermore, unawareness of this plurality of perspectives on motor learning can hinder the development of both original knowledge and innovative practices (2,3). This leads us to address a second question: ‘How do we (re-)learn motor skills?’.
Traditionally, the concept of learning a new motor skill has been associated with the idea of acquiring a new motor program internally stored in the brain. The most well-known version of this approach is the Generalized Motor Programs (GMP) theory developed by R. Schmidt (4). This cognitive approach of motor learning has been prospering in the modern literature through studies focused on reinforcing the acquired knowledge stored in cognitive schemes – or mental representations supported by memory processes – to achieve automaticity in expert gestures. This research question particularly raised the notion of repetition as a key point in the traditional view of motor learning. Within this framework, novice performers can repeatedly mimic the one “correct” technique that all experts share to acquire and reinforce a new motor skill.
According to Kamm, Thelen and Jensen (1), this cognitive motor theory has dominated the study of learning for two main reasons. First, this research area originated from questions about the relationship between the brain and behaviour, which shifts the focus onto the role of the brain in the learning process. Second, theories of motor learning evolved simultaneously with our advancing understanding of the brain.
However, the correct, gold-standard technique achieved by reinforcing cognitive programs through repetition is not the only existing approach to understand motor learning. The ecological dynamics approach of motor control, largely inspired by the pioneers J.J. Gibson (5) and N. Bernstein (6), offers an alternative view of learning and expertise.
Gibson’s research (5) emphasizes that the behaviour of an agent can only be understood in relation to the environment in which it occurs, and thus by considering the agent-environment system as the fundamental, inextricable unit of analysis. His concept of affordances – i.e., opportunities for action offered by the environment that are specific to an agent’s capabilities – was formulated to evidence this agent-environment mutuality through action-scaled measures (i.e., ratios of agent characteristics to environment features). In other words, action possibilities (e.g., such as walk-ability, climb-ability, sit-ability, catch-ability) are directly perceived in terms of fits between the agent and the environment.
This ecological approach of motor behaviour has been enriched by incorporating dynamical aspects in the study of perception-action couplings. This extension was primarily inspired by Bernstein’s research (6), which showed how the numerous degrees of freedom within the body (i.e., inherent variability arising from many muscles and joints) can be organized into functional, temporarily constrained coordinative units – called synergies (7) – to efficiently exploit variability in the agent-environment system when solving task-specific motor problems.
Rather than a sophistication of acquired cognitive processes, expert performance can thus be described as an improved fit between the agent and environment – or, in Gibson’s terms, as an expanded field of affordances. Instead of depicting the expert as an advanced human-machine capable of executing and replicating an error-free technique, Bernstein introduced the concept of “repetition without repetition” to emphasize that variability should not be considered as noise to be minimized, but rather as an essential feature of biological organisms, inherently and inevitably involved in the learning process. In this view, experts can be defined as agents who exhibit a great ability of mastering the numerous degrees of freedom within the body, which allows them to adapt to individual, task and environmental constraints when solving specific motor problems (8). Experts are self-organized problem solvers, who established coordinative structures among degrees of freedom (or synergies) to efficiently exploit the variability present in the environment-actor system (9).
To sum up, Gibson’s and Bernstein’s work gave rise to an alternative conceptual framework of motor learning, where the learner’s coordination dynamics evolve towards forming coordinative units (or synergies), which themselves emerge from exploring perception-action couplings through task-specific interactions between the agent and environment (10).
In the present Toolbox, we employed the term “systems perspective” in line with these ecological dynamics approach of motor learning, where 1) behaviour emerges from complex interactions within the agent’s body system at one scale and within the agent-environment system at another scale, and 2) movement variability has a functional role in exploring these interactions when learning a motor skill. In rehabilitation, the aim of helping patients with motor disorders can thus be reformulated from a systems perspective as guiding them to discover new coordinative movement solutions, thereby expanding their action capabilities within their environment through re-learned perception-action couplings.
With the concepts of rehabilitation and the systems perspective now defined, we can examine to what extent rehabilitation in sports injuries has been approached from a systems perspective. In this brief report, this question will be addressed based on 1) a literature review, which provides a comprehensive understanding of how a systems perspective has been used in research to develop both clinical assessment and intervention, and 2) a secondment in clinics, offering insights into how a systems perspective can be applied to clinical practice. To better illustrate our discussion points, different injuries occurring in various sports will serve as specific examples. Because the present Toolbox primarily aims to capture the ongoing dialogue between academic and clinical fields, we will conclude with some recommendations for building the necessary translation bridge to improve rehabilitation and, ultimately, enhance patients’ quality of life.
PART 1 [Literature Review]:
To what extent sport injuries are approached from a systems perspective in research?
The first part of this Toolbox examines the extent to which a systems perspective – as defined earlier by its incorporation of complex interactions and movement variability within the agent’s body system at one scale and the agent-environment system at another scale – has been integrated into the scientific literature on sports injury rehabilitation. While the importance of research-driven rehabilitation is widely recognized, the use of a systems perspective remains marginal, or at least, limited. Research in ACL rehabilitation clearly illustrates this statement. Indeed, the role of ACL in knee stability was first studied in the period of 460-370 BC and its deficiency has been a major focus of research over the last five decades, especially with the development of surgery, technology, and biology (11–13). Nevertheless, the current ACL rehabilitation techniques are still controversial or present a very little scientific evidence for their validity (14–17). Moreover, re-injury often occurs, in half the cases in the contralateral limb because of non-contact mechanisms (18). This observation may likely be the consequence of reducing the complex phenomenon of ACL injury into a sum of damaged structural elements and isolated risk factors (19–21).
Yet, pioneering attempts to apply an ecological dynamics approach of motor learning to motor disorders originated from the 1980-90s (1,22–25). Several tools and practical guidelines were developed to bridge the gap between clinical practice and research supporting a systems perspective in rehabilitation.
1.1 Clinical assessment tools inspired from a systems perspective
1.1.1 The Environment-Athlete System: action-scaled measures
Among the methods proposed to assess clinical outcomes from a systems perspective, action-scaled measures have been suggested to inspect mismatches between the agent and environment, enabling the design of interventions based on agent-environment units, rather than on external biological standards (26). Such mismatches can thereby be studied using the Gibsonian concept of affordances, as well as through biomechanical models that consider both the effectiveness and energy cost of the movement solutions exhibited by the patient (27).
For example, an affordance-based methodology – the PACT metric which quantifies perception-action coupling behaviour – has lately been proposed to assess return-to-play readiness after sport-related concussion (28). While concussion has historically been considered using a “one-size-fits-all” approach (i.e., homogeneous diagnosis and treatment across all individuals), this methodology acknowledges that examining perceived affordances (which are individual-specific) can improve the accuracy of clinical assessment. Indeed, it was found that a disrupted perception-action coupling was exhibited by concussed athletes who are yet recovered according to standard clinical norms. This finding led to a theoretical model depicting the relationship between sport-related concussion and dysregulation of perception-action coupling (29), which highlights how restoring a coupled athlete-environment system may reduce the risk of musculoskeletal injury upon returning to the field. For example, the ability of perceiving “passability” affordance through a gap between two approaching defenders is crucial for rugby players (30), and should therefore be assessed as a return-to-sport criterion after cerebral concussion.
Action-scaled measures arise from the assumption that non-standard movement patterns are not necessarily pathological, and that impairments are just one type of constraint added to the self-organized agent-environment system, which seeks an optimal solution to the motor problem it faces. It is then the therapist’s mission to estimate whether these patterns may lead to undesirable long-term consequences. If they do, the therapist can intervene to guide the system towards more adaptative movement solutions, using techniques that assess coordination dynamics.
1.1.2 Coordination dynamics: HKB landscape and coordination profiling
In the view of synergetics (7), the information exchanged between the nonlinearly interacting parts of a system can be compressed at the macroscopic level into a collective low-dimensional variable called order parameter. This higher-order variable captures a movement solution at the behavioural scale. Using the Haken-Kelso-Bunz (HKB) model (1985) (31,32), the order parameter’s dynamics can be illustrated in a dynamical landscape defined by a potential function – i.e., a topology of the behavioural repertoire with more or less stable solution patterns. In this landscape, behaviour is pulled towards attractors of a certain stability represented by wells. This dynamical landscape can be altered by the manipulation of key variables called control parameters, which drive movement pattern transitions when reaching critical values.
In rehabilitation, methodological recommendations have been proposed to map and act on the patient’s dynamical landscape (1,7,23,24). Derived from a dynamic view of motor learning, this landscape tool allows tracking behavioural changes, such as the emergence of new coordination patterns or a greater ability to switch between patterns, taking advantage of the body system redundancy in a given context of constraints and possibilities. Beyond clinical assessment, the use of dynamical landscapes can guide constraints manipulation when helping patients discover functional movement solutions (please refer to Subsection 1.2.2. for more details on designing therapeutic interventions using the patient’s dynamical landscape).
This methodology born from a nonlinear complex system approach can particularly be applied to sports injury forecasting (33,34). Using the core concept of self-organization of a systems approach, sports injury can be conceptualized as a complex, emergent phenomenon. Instead of using linear tools to identify causality relationships between isolated risk factors and injury occurrence, a systems approach aims to identify and track the time evolution of a meaningful order parameter that can capture the athlete’s dynamics in response to training and competitions. Once the dynamics of the order parameter is captured, the next step is to identify the changes that signal an upcoming transition in athletes’ behaviour. Sports injury can thereby be forecasted as a phase transition preceded by increased fluctuations in the athlete’s dynamical landscape (34).
In clinical assessment, the relative phase between the angular displacement of joints or segments has been identified as a relevant order parameter to differentiate various pathological conditions from healthy individuals. To cite some examples, the pelvis-trunk coordination of runners with moderate or recovered low back pain exhibited a greater in-phase pattern in the transversal plane compared to healthy controls, and a decreased coordination variability was also indicative of pathology (35). Similar results were found in a pioneering study that applied a dynamical systems approach to running injuries, evidencing lower relative-phase variability in individuals with patellofemoral pain compared to healthy subjects (36).
As another example, alterations in inter-joint and inter-segment coordination have also been detected in patients with ACL injury (very common injury in sports involving cutting manoeuvres such as team sports and skiing) by various studies using relative-phase measures (37–41). In complement, coordination profiling with clusters and PCA analyses has also been suggested as a qualitative assessment method in sports medicine (42) and ACL injury (43,44).
To cite some examples of altered coordination in ACL patients, the excessive rigidity found in their hip-knee coordination – i.e., lower relative-phase variability compared to healthy controls – was interpreted as a pathological behaviour, because it reduces the postural system adaptability to perturbations and because the repetition of a single coordination pattern exerts persistent load on a restricted area, which can lead to structural damages and functional complications on the long-term period (41). Also, the abnormally great in-phase pattern found in the knee-ankle coordination of ACL patients increases the risk of re-injury, due to an exaggerated knee valgus combined with ankle inversion when the coordinated movements of these joints are executed in the same direction.
These illustrative scenarios of excessively rigid coordination patterns highlight the need of developing coordinative solutions during ACL rehabilitation (please refer to the Subsection 1.2. for more details). Moreover, they suggest that another approach to finding order parameters candidates for clinical assessment would be to examine the variability structure in the athlete’s movement time series.
1.1.3 Variability structure: nonlinear analyses
In the late 1980s, the researchers Goldberger and West, respectively specialized in Medicine and Physics, multiplied collaborative studies to develop a dynamical theory of health and disease, which claims that complexity is inherent to healthy biological systems (i.e., functional systems adaptable to perturbations) and that decomplexification is a common feature of pathological systems (i.e., non-functional systems vulnerable to perturbations) (45–47). Based on related findings on various pathological conditions, Goldberger and Lipsitz (48) described this loss of complexity as “(i) a loss or impairment of functional components, and/or (ii) altered nonlinear coupling between these components”. While the approach traditionally adopted in clinics use linear models to identify the absence/presence of abnormalities in isolated organ systems, this alternative theory aims to assess the functionality of the body through its level of complexity, where complexity “arises from the interaction of a myriad of structural units” (48). This approach and derived theories based on the same conceptual framework (49,50) have inspired the contemporary literature to revise the concept of pathology, as well as the techniques used for clinical assessment, prevention and intervention.
In this view, nonlinear measures – including entropy measures, the largest Lyapunov exponent, fractals, dimensional analysis and detrended fluctuation analysis – are particularly relevant for studying human movement, which emerges from nonlinear dynamical interactions. Whereas linear measures are useful for quantifying the magnitude/amount of variability in a movement time series, nonlinear measures can reveal a complexity index of behaviour by unmasking the “subtle, hidden temporal structure” of movement variability (51). A nonlinear approach acknowledges the presence of chaotic temporal variations that are inherent to healthy biological systems, functional in the sense that they are able to adapt to changing constraints (48).
In sports injury, nonlinear analyses have notably been used to detect a loss of complexity in patients with ACL injury, depicted as alterations in both spatial and temporal patterns. For instance, tibial fractal signatures were found to be greater in both uninjured knees and uninjured individuals compared to ACL-deficient knees, indicating decreased bone architecture complexity in the latter (52). Altered patterns following an ACL injury were also reported in studies focused on behavioural dynamics (53). In a study assessing quiet stance, the nonlinear dynamics of centre of pressure were extracted by recurrence quantification analysis in ACL-deficient patients, whose oscillations were found to be significantly more regular than those of the healthy controls (54). In gait studies, entropy analyses revealed excessive periodic patterns in stride-to-stride variability of the ACL-deficient knee compared to the contralateral knee (55) and to healthy controls (56), and that this rigidification of gait behaviour gets intensified one year after rupture (57). In summary, fractals and entropy can respectively detect spatial and temporal excessive periodicities/regularities in pathological populations such as injured athletes, while healthy individuals exhibit a functionally organized variability.
Importantly, the selection of assessment methods after sports injury can lead to different clinical interventions, that might be inadequate if neglecting some important aspects of sway variability. For example, it was found that the structure of postural oscillations was not fully restored in athletes after cerebral concussion, as healthy controls exhibited less periodicity in their postural oscillations (58–60). Yet, similar sway amplitudes and acceptable equilibrium scores encouraged return-to-sport, disregarding the abnormal rigid behaviour in athletes. These studies were extended onto the long-term period, demonstrating that, although the amount of sway variability was restored one month after the concussion, a 3-month postinjury period was insufficient for athletes to regain a postural sway as complex as healthy controls (61). Therefore, nonlinear measures help better identify structural changes after a sports injury, allowing for an effective rehabilitation plan focused on functional recovery, and therefore prevent re-injury due to a premature resumption of sport and physical activities.
1.1.4 Systems-based tools for (re-)injury prevention
Given the importance of complexity in functional biological systems, epidemiological research should be broadened from a systems perspective with the use of terminologies and analytical tools from the field of nonlinear sciences (62). In this sense, efforts have notably been made to develop systems-based preventive methods for ACL injury (63). While reductionistic tendencies have been reported in ACL prevention research, an alternative conceptual and methodological framework based on the combination of in vivo, in vitro and silico techniques were proposed to better understand the complex relationships between joint biomechanics and joint injury mechanisms (21). A paradigm shift from a reductionistic to a complex systems approach for preventing ACL injury was later encouraged by introducing a novel systems-based model (19): “Since injury is a complex phenomenon characterised by uncertainties and inherent non-linearity, an ACL injury will emerge when a specific pattern of interaction happens in the presence of an inciting event of a given value. Thus, the best manner to predict an injury is by understanding the interactions among the web of determinants and not the determinants themselves.” Additionally, ACL (re-)injury prevention should consider the use of neural networks, classification and regression trees (CART) and machine learning tools relying on probability computations that can take into account the nonlinear nature of the relationships between injury determinants – rather than the use of linear tools relying on the causality relationship between an isolated risk factor and the occurrence of injury. In a similar vein, a recent study provided some illustrative techniques based on a complex systems approach to help clinicians assess readiness for return-to-sport after ACL injury (64).
Finally, the incorporation of a systems perspective into rehabilitation also allowed the revision of some conventional return-to-sport criteria that reduce the complex alterations following ACL injury to a one-leg problem (e.g., limb symmetry indexes) (65–67). Similarly, systems-based clinical interventions were proposed as an alternative to reductionist practices.
1.2 Clinical interventions inspired from a systems perspective
1.2.1 Affordance training
Because injured athletes with acceptable clinical standard outcomes may still present a disrupted perception-action coupling, affordance perception (please refer to Subsection 1.1.1.) should not only be assessed with action-scaled measures but also trained before return-to-sport. In this sense, the ecological dynamics framework offers an effective approach to understanding and preventing contact injuries in invasion team sports (such as football) by examining the interactions within the attacker-defender-environment system (68). This systems perspective highlights how information constrains the interactions among competing players and the ball, and notably those which enhance injury risks. In contrast with linear causal approaches that rely on indirect preventive methods (e.g., referees firmly prioritizing player safety over player engagement), this affordance-based approach aims to educate players to detect high-risk situations through active learning. To do so, it employs the HKB framework (please refer to Subsection 1.1.2. for more details) to identify threshold values of critical control parameters (e.g., interpersonal distance, displacement velocity; (69)) that drive the opponents-ball system to the state of injury. Therefore, the incorporation of a systems (ecological dynamics) approach into both preventive training and return-to-sport programs to help athletes detect affordances that specify high-risk situations, and, in turn, enhance decision-making skills and movement adaptability to prevent (re-)injuries. In boxing, for example, a study described how adaptable movement patterns emerged from the perception of “harmability” (i.e., affordance specifying risk injury), without additional instructions from a coach or referee (70).
Moreover, virtual reality (VR) environments have been proposed as an athlete training solution whose implementation should be guided by an ecological dynamics approach (71). The design of affordances in these virtual learning environments should ensure that the presented informational constraints are faithful to the athlete-environment system and are specific to relevant sport situations (task-specific) – for example, perceiving gap “passability” affordance in rugby (29,30) or football (71) should be practiced. One advantage of VR in the rehabilitation process is that action fidelity (faithfulness actions-responses) can be reduced and gradually adjusted to facilitate a safe return-to-play while minimizing the risk of reinjury.
Another benefit of VR is that affordances can be designed and manipulated to guide the athlete in exploring various relevant information variables and movement solutions – and thus, promoting re-learning through diverse athlete-environment interactions. An implementation of an ecological dynamics approach into virtual (re-)learning environments therefore emphasizes the design of affordances under various informational constraints to stimulate problem-solving behaviours and, in turn, encourage the exploration and development of a wide, creative, and individualized movement repertoire. In other words, constraints manipulation is a key element in implementing a rehabilitation plan based on a systems (ecological dynamics) perspective.
1.2.2 Constraints-led approach (CLA)
As mentioned above, designing clinical interventions from a systems perspective can consist of encouraging movement exploration through constraints manipulation, rather than prescribing specific movement patterns considered to be optimal according to standard norms (1,2,23–27,72–74). Re-shaping performer, environmental or task constraints is necessary to destabilize the current dysfunctional solution and help discover of a healthier one. This approach is also known as the constraints-led approach (CLA). In sports injury prevention, manipulating task constraints has notably been proved to be an effective motor learning method for reducing the risk of ACL injury (75,76).
Using HKB terminologies (please refer to Subsection 1.1.2. for more information), the therapist’s job is to identify control parameters through constraints manipulation in the patient-task-environment system, and to carefully adjust them to elicit a qualitative change in the order parameter. Thirty years ago, Wagenaar and van Emmerik (1996) were already stating: “The key assumption in these approaches is that movement disorders are not only the consequence of structural abnormalities but can also be understood as an abnormal spatio-temporal organization in the perception-action coupling and in movement coordination; qualitative changes can be brought about by the interplay between control and order parameters of the system.” (24) (p. 173). To put it differently, manipulating informational constraints can induce phase transitions in patients and drive them to a meta-stable dynamical landscape (i.e., with multiple movement solutions), underpinning the emergence of innovative, creative behaviours. Therapists can therefore be viewed as “change agents” (25) (pp. 51, 52), whose the role is to guide patients in their search for new, more functional, movement solutions. In addition to CLA, other systems-based interventions – such as differential learning – have been proposed in the literature to promote movement exploration in sports injury rehabilitation.
1.2.3 Differential Learning (DL)
Given the uniqueness of movement patterns both across performances in a repeated task and across individuals, traditional repetition-based training methods and group-based exercise prescriptions have been questioned. Based on the theory of dynamical systems, the Differential Learning (DL) method considers learning as a self-organizing process where amplifying stochastic perturbations destabilizes the body system and encourages it to explore a large diversity of solutions for reaching the task goal (77,78). In other words, DL aims to enhance movement fluctuations to promote metastability in the learner’s landscape (for more details, please refer to Subsection 1.1.2.), thereby encouraging the discovery and switching between new movement solutions.
While CLA encourages variability in practice to guide the patient’s search for individual movement solutions, DL takes a more radical stance on the functional role of variability in the (re)learning process by requiring patients to experience as many movement solutions as possible. Importantly, DL interventions avoid movement repetitions and corrective instructions are provided in DL – in contrast to classical methods, which consider deviations from gold-standard patterns as erroneous movements.
In a recent study, DL was shown to be more efficient in reducing the risk ACL injury compared to methods based on prescribing the ideal pattern of movement with demonstration, imitation, repetition and correction (79). The importance of movement variability in preventing ACL injury was further supported by another study (75), which however recommended guiding learners to adapt to manipulated task and environmental constraints (i.e., CLA), rather than adding random and imposed (not self-regulated) variability during movement exploration (i.e., DL). In sports injury rehabilitation, DL-based interventions may be particularly effective in promoting movement diversity in athletes suffering from repetitive strain injuries (e.g., tennis elbow caused by repetitive gripping, runner’s knee due to repeated ground impacts, or rotator cuff tendonitis due to repetitive paddling or ballistic movements in swimming, surfing, or baseball, to name a few) (77). In these clinical situations, the benefits of DL extend beyond promoting re-learning through movement exploration and adaptability; they also encourage the development of complex, whole-body movements.
1.2.4 Whole-body movement exercises
The previous paragraphs reviewed how the problem of degrees of freedom (DoF) posed by N. Bernstein (6) has recently been applied into sports rehabilitation. Instead of prescribing patients a gold standard movement to reproduce, clinicians are encouraged to promote variability in their rehabilitation programmes so that patients can better explore the task solution space when re-learning a motor skill. This active exploration leads to an enhanced ability to cope with a greater number of DoF. Enriching movement coordination repertoires is functional, as it allows the emergence of adaptative solutions regarding post-injury individual constraints, as well as an increased adaptability to balance perturbations with a reduced risk of re-injury (75).
Besides encouraging movement variability, therapists can design clinical interventions from a systems perspective by encouraging interactions in tasks involving a high number of degrees of freedom, such as whole-body movement exercises and Tai Chi (80,81). In sports medicine, biomechanical insights into force dissipation across multiple joints through kinetic chains have led to an improved version of an ACL rehabilitation exercise (20). This systems-based intervention involves the trunk, pelvis and hip muscles in a three-planar manner to control the dynamic knee valgus (DKV), often involved in ACL injury. This effort into engaging the body “as a whole” in ACL interventions was further supported by another study (67), where the unilateral cueing “do not let your ACL knee roll inward when landing” was replaced by the task “reach both knees towards the cones in front of you when landing”. Beyond the benefit of engaging both injured and uninjured knees in the task, a subsequent review emphasized how improving postural stability in ACL patients was better achieved when providing instructions related to the task (e.g., “try to minimize movement of the bars on the balance board you are standing on”) compared to instructions related to specific limb segment positions (82). Finally, this consideration of an injured-uninjured system can be extended to the interpersonal scale.
1.2.5 Inter-agent training: from Complexity Matching to Joint Action
The concept of engaging the body as a whole during rehabilitation has been extended to the interpersonal scale. The idea of restoring complexity in pathological individuals through interpersonal coordination trainings with healthy pairs has notably been explored by testing the Complexity Matching hypothesis (83) as an original systems-based rehabilitation method. According to this hypothesis, a pathological (decomplexified) system should restore its complexity by maximizing information exchange with a healthy (complex) system. In practice, it was applied into the design of trainings where younger and older agents were mechanically coupled (i.e., arm-in-arm walking). To our knowledge, the Complexity Matching hypothesis has never been explored in sports injury rehabilitation, although it delivered convincing results in terms of postural stability improvement (84,85).
While it would be interesting to test the efficiency of a Complexity Matching training in populations with sports injuries, side-by-side coupling does not beneficiate from the shared-goal nature of Joint Action. Joint actions are commonly observed in everyday life, whenever two or more agents coordinate their actions to reach a common goal (e.g., shaking hands, navigating on a crowded street, jointly moving a dinner table). From a Bernstein’s perspective, one could expect that informational and/or mechanical couplings in joint-action tasks should reduce the great dimensionality of DoF – i.e., the system elements (body parts at the inter-limb scale, agents at the inter-agent scale) should be constrained to behave as a single unit through the couplings implied by the task jointly performed. Such a dimensional reduction may have a particular clinical interest, as it should lead the uninjured and injured elements to re-learn how to move as a whole.
To clarify, while movement variability should allow injured athletes to discover adaptive solutions in response to balance perturbations, dimensional reduction should foster coordination efficiency by organizing these redundant DoF into stable, low-dimensional, functional units – also called synergies. Moreover, synergies are also characterized by reciprocal compensation between the system elements. By virtue of its inherent principles of dimensional reduction and reciprocal compensation, interpersonal synergies (86) through joint action should help injured athletes re-learn perception-action by “moving just as one” with their healthy teammate, whose structural and behavioral complexity is intact.
Recently, REPAIRS investigated the potential clinical benefits of joint action using coordination and synergy analyses (87), offering promising insights for ACL rehabilitation. To our knowledge, joint-action tasks involving both pathological and healthy partners have not yet been explored using coordination analyses, although such tasks may be particularly relevant for rehabilitation – particularly in the context of sports injury recovery. The first part of this Toolbox outlined various methods and research directives from the literature aimed at advancing sports injury rehabilitation from a systems perspective. To further address this question, the following part examines the extent to which this systems approach is implemented by therapists working with patients recovering from sports injuries.
PART 2 [Secondment in Clinics]:
To what extent sport injuries are approached from a systems perspective in practice?
The second part of this Toolbox presents insights drawn from both observations and interviews conducted during a two-week secondment at the R’Equilibri_us clinic (Portugal, Lisbon). Although it may not be representative of all rehabilitation practices, this secondment provided a first glimpse into the dialogue between researchers and clinicians – and particularly regarding the practical application of knowledge developed from a systems perspective.
This section draws on several clinical situations observed during the secondment, which are described below to illustrate key points. Additionally, two physiotherapists participated in a 30-40-minute semi-structured interview focusing on both translational and systems-perspective aspects. Rather than conducting statistical analyses on a limited dataset, the information gathered through observations, informal discussions and interviews was used to present a range of – sometimes converging, sometimes diverging – examples of rehabilitation professionals’ interests and intervention techniques related to motor learning.
To better organize its outcomes, the secondment was designed to address two main dimensions:
1) Translation (i.e., how is the dialogue between researchers and clinicians), and
2) Systems Perspective (i.e., to what extent clinical practices are based on a systems perspective).
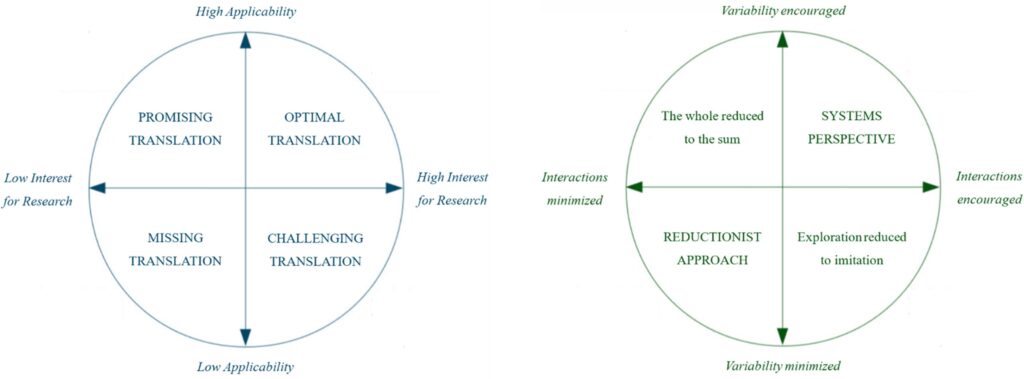
Each dimension can be structured as a circular diagram with a horizontal axis and a vertical axis (Figure 1).
For the Translation diagram, the axes were:
– Interest for Research (e.g., low or high scientific activity through reading literature, attending workshops and conferences, searching for scientific findings and updates), and
– Applicability (i.e., low or high difficulty to translate knowledge into practice).
For the Systems Perspective diagram, the axes were:
– Interaction (e.g., rather assessing the patient’s abilities in relation with the environment or using external standard norms, rather conceptualizing the body as a system with complex nonlinear interactions or as a sum of isolated structures, rather encouraging exercises involving multiple degrees of freedom such as coordination activities or restricting the re-learning process to exercises exclusively focused on the injured area), and
– Variability (e.g., rather conceptualizing variability as an index of functionality or as noise to be minimized, rather encouraging the exploration of multiple movement solutions or prescribing an ideal movement pattern to reproduce).
2.1 A challenging research-clinic translation
| Extracts from the interview with Physiotherapist A: How important is the role of research in rehabilitation, according to you? “It should be a priority to keep on developing research to make sure that we’re getting the results that we want. […] I think it’s also important to make sure we connect that with evidence-based practice, patient experience, healthcare professional experience. So, I think that we have to encompass all those concepts. But research leads the way in terms of what we want to do better and how we get there.” As a physiotherapist, how would you describe your own relationship with the research area? “It’s a mixed relationship. […] I tried to start reading research very early on when I was a graduate student. And that got me really interested personally […] I knew how important it would be in practice later on. So, my personal experience with it is that it’s very important to keep in touch with the concepts and the guidelines that are relevant to the clinic. […] On a more negative side, I do find it hard to select what’s important in research because a lot of stuff comes up. And I think that we have to be very careful to select what matters to us from a clinical aspect. […] And still, even if you try to read research related to your clinical practice, you need to be up to date with the best way to treat an ACL injury, the best way to treat muscle injuries, whatever. So, it’s hard. It’s hard to keep up to date with so much research that’s coming up. So, it would be a challenge, I would say.” How good or how bad do you feel the dialogue between researchers and clinicians is? “I think that a lot of research can just become completely disconnected from the real world, the real-world life settings […] I have time constraints – about how much time I can read research – so I need to understand very clearly what can bring some value to my patients and to me as a clinician […] Having some contacts with the real world should allow researchers not to be disconnected from it”. We figured out that we both went to a common workshop on movement variability. Once you get out of such workshop, what’s the next step in the clinic? Do you feel it’s easy or rather difficult to implement this knowledge into practice? “[…] Historically, physiotherapists have been very corrective in terms of movement. […] For example, for a shoulder injury, you may ask to move in a very specific way, to bring your shoulders back, bring your scapula down […] Understanding that variability is fine, that it is healthy, and that you need a lot of movement strategies to deal with the environment around you and daily tasks… so just applying that general idea to my clinical reasoning and practice was quite easy. […] I implemented things a bit differently in the clinic: how do you restrict not the person but the environment around the person, without trying to be too limiting to the development of new movement strategy? So, the general concept is easy to integrate into clinics. However, when it comes to bring a very analytical movement analysis into practice, I think it can still be quite challenging.” Extracts from the interview with Physiotherapist B: You told me once that you read the scientific literature every day, is that right? Can you tell me more about your interest in research? “Yes, I read every day. I have a special interest in the area of pain, because pain is the main problem that people report to us – physiotherapists – and I have as well a special interest in neuromuscular aspects in strength training or exercise, because there is evidence that exercise is the first-line option for all the conditions we encounter in clinical practice.” How often does something you read inspire you to create a new exercise or modify your approach in clinical practice? “It happens a lot. I like to learn, I think it’s very important to adjust the way I do my job. And I think I can grow up as a better professional. […] However, sometimes it’s very difficult to check which studies are good or important, if they have good quality or not, and if they have some impact on my clinical practice.” In your view, what efforts could be done to improve communication between researchers and therapists? “In Portugal, at this moment, our professional body – Ordem dos Fisioterapeutas – has a subgroup whose job is to listen to physiotherapists working in practice and to collect their needs regarding research. The idea is to ask physiotherapists what can be done in research to help them in their practice. In Portugal, I think we have around 10,000 physiotherapists, but only about 300 responded to the survey. So only a small part responded. I think it’s very useful to have this kind of channel – ‘I’m in practice, you’re in research’ – so we can collaborate. We need to ask: ‘What can I do for you, and what can you do for me?’. We need to share, support each other, and build that connection. Another idea is that we can also talk with universities – same thing.” |
Table 1 presents the perspectives of two physiotherapists from the R’Equilibri_us clinic on the importance and effectiveness of the current dialogue between research and clinical practice. To sum up, both therapists recognized the critical role of research in rehabilitation, emphasizing that it should guide better clinical outcomes and support evidence-based practice. Both showed a strong interest in incorporating scientific knowledge into the development of new and improved exercises.
However, they highlighted several challenges in translating research into rehabilitation, including too much information, difficulty judging study quality, and instances of disconnect between research and real-world practice. While some general concepts from the literature can be easily applied, it remains challenging to incorporate research-based movement analysis into daily clinical practice.
Beyond their specific clinic, efforts are underway in Portugal to connect research with practice, even though interviewees emphasized the need for improving even more collaboration between researchers and practitioners (e.g., “We need to share and build that connection”).
2.2 Varied approaches to sports injury rehabilitation
During this clinical secondment at the R’Equilibri_us clinic, fifteen patients suffering from various sports injuries were observed during rehabilitation exercises (Table 2). Some of these exercises were largely inspired by a systems perspective, while others could not be fully understood within this framework. One aspect of the systems perspective that was, however, consistently considered throughout was the idea of tailoring learning experiences to the unique needs, abilities, and motivations of each patient. This patient-centred approach is rooted in the systems perspective described earlier, as it reflects the inherent complexity and non-linearity of rehabilitation, where the same injury can lead to very different relearning behaviours across individuals.
All physiotherapists at the clinic gave a particular attention to this approach, explicitly stating: “Two patients may present with the same injury, at the same time post-surgery, in the same clinic, yet their completely different profiles lead to different exercises”, or: “I don’t treat a knee injury, I treat a patient with a knee injury”. The diverse range of exercises performed by the seven patients with ACL injuries further illustrates this point. Let’s take a closer look at Patient 8 and Patient 9 to describe how this patient-centred approach was employed at the clinic.
| Patient | Sport | Injury | Rehabilitation State | Sport Profile / Aim |
| 1 | Tennis | Sprained Ankle | 1st day (assessment) | Tennis Club. /Initial aim: Participate to the next competition. |
| 2 | Skateboarding | Sprained Ankle | 6 months, back to sport already | Skateboarding as lifestyle. /Skate more again. |
| 3 | Ballet | Chronic Tendinopathy (both lower limbs, patellar surgery) | 6 months before surgery 3 months after surgery | Ballet Company, Overtraining. /Back to ballet in 2 months |
| 4 | High Jump | Meniscus Tear | 2 weeks before surgery 3 days after surgery | Physical Education course, out-of-school unspecified. /Aim unspecified. |
| 5 | Jiu-Jitsu | Meniscus Tear | Post-surgery (period unspecified) | Other sports like surfing. Back to Jiu-Jitsu Club. /Accompany RTS with in-clinic rehabilitation. |
| 6 | Basketball | ACL Injury (first rupture, weighing pros and cons of surgery), Meniscus Tear | 3 weeks | Basketball Club. /Return to sport (RTS) as soon as possible (ASAP). |
| 7 | Motocross | ACL Injury (first rupture, no surgery) | 2 months | Riding as a hobby. /Aim unspecified. |
| 8 | Taekwondo | ACL Injury (first rupture, with hamstring graft) | 7 weeks after surgery | Other sports (university) /Aim unspecified, fear of reinjury. |
| 9 | Running | ACL Injury (first rupture, with hamstring graft) | 6 weeks before surgery 8 weeks after surgery | Into various sports /Play tennis in 2 months, Marathon in 3 months. |
| 10 | Football | ACL Injury (first rupture, with meniscal surgery) | 3 months before surgery 5 months after surgery | Football Club. /RTS ASAP. |
| 11 | Football | ACL Injury (second rupture, hamstring graft, then patella graft) | 4 months before surgery 5 days after surgery | Football Club: First sport injury at 15 y-o. /RTS ASAP. |
| 12 | Football, Rugby | ACL Injury (third injury on the same knee, second surgery: allograft), Meniscus Tear | 8 months before surgery 4 months after surgery | Incomplete rehabilitation for a sprained knee before two successive ACL tears. /Focus more on coaching. |
| 13 | Padel | Knees Cartilage and Upper-Arm Injury | 1 year | /Aim: Keep on playing while managing pain. |
| 14 | Padel | Elbow Injury | Unspecified | Unspecified. |
| 15 | Jiu-Jitsu | Shoulder Injury (acromioclavicular joint) | 2 months (late start: 1 year after injury) | Unspecified. |
Patients 8 and 9 share several profile characteristics, including the nature of their injury (i.e., a first-time ACL rupture), their surgical choice (i.e., hamstring graft), their stage in rehabilitation (i.e., approximately two months post-surgery), and the importance of practicing various sports in their daily lives (Table 2). Despite these similarities, the physiotherapists maintained that a one-size-fits-all approach (i.e., applying the same treatment to the same type of injury) would be inadequate to effectively support these patients in the rehabilitation process. For example, the fear of reinjury expressed by Patient 8 was not (or at least not as strongly) palpable in Patient 9 who, in contrast, had discontinued the use of crutches the previous month and articulated ambitious sporting challenges for the upcoming months. This results in differing relearning paces and the implementation of individualized rehabilitation exercises, as clearly stated by a physiotherapist of the clinic: “At early stages, we may aim for similar objectives across patients, such as managing pain and removing crutches; but how you get there and when you’ll get there depends on who stands in front of you”.
For example, Patient 8 cautiously began practicing a one-legged step-down, with the physiotherapist offering encouragement to address the patient’s lack of confidence during the exercise. In contrast, Patient 9 performed step-up and step-down exercises while holding weights, paying little attention to the physiotherapist’s presence. While Patient 8 focused on localized reinforcement exercises using an elastic band around the lower limbs, Patient 9 engaged in various weight-lifting exercises (e.g., trunk rotations with bent knees while holding weights, one-legged sit-to-stand movements with weights, lifting weights from the ground with one leg extended). Additionally, all of Patient 8’s exercises were performed on a firm surface, whereas Patient 9 also trained balance on unstable surfaces and practiced trampoline jumping.
Furthermore, the importance of adopting a patient-centred approach in clinical practice was supported during the interviews, as shown in Table 3 (e.g., Physiotherapist A’s response to the second question; “The person always comes first. They dictate where the treatment goes”).
Beyond the variety of rehabilitation exercises, the patient-centred approach applied in the R’Equilibri_us clinic was also evident in the way physiotherapists consistently informed patients of the available options, including their risks, benefits, and trade-offs, while ultimately allowing patients to decide which rehabilitation paths best suited their needs. For example, the exercises proposed to Patient 9 were adjusted to align as closely as possible with their sporting goals, although these goals were considered by the physiotherapist to be overly ambitious. To do so, exercises that would have been too premature given the patient’s ligament vulnerability were prescribed within an outpatient aquatic program, where force constraints are significantly reduced. On the other hand, discussions with the physiotherapist helped Patient 1 reconsider their initial objective of participating in the upcoming competition (Table 2), which would have posed a very high risk of reinjury. In addition, the physiotherapists provided general and tailored warm-up exercises to support any patient who aimed to return to sport as soon as possible. Just as the return-to-sport decision emerged from dialogue between both the patient and physiotherapist, surgery options were presented in detail to provide the patient with informed guidance and support, rather than binary instructions. For instance, at an early stage of rehabilitation, Patient 6 appeared uncertain about whether to undergo surgical intervention following a first ACL rupture or to continue with non-surgical treatment (Table 2). To further support Patient 6, the physiotherapist recommended consulting the decision aid website for ACL injury treatment https://www.aclinjurytreatment.com/, developed by university professor S. Filbay. The platform aims to inform patients about current treatment options, compare likely outcomes based on each approach, outline respective pros and cons, and provide a questionnaire to help patients identify the option that best aligns with their individual needs and expectations (Please note here that this decision aid also serves as a valuable example of knowledge translation. By integrating it into their practice, the R’Equilibri_us physiotherapists helped strengthen the connection between their patients and the researcher who developed the tool using an evidence-based approach in collaboration with clinicians, with the explicit goal of making it accessible and user-friendly for patient).
| Extracts from the interview with Physiotherapist A: You just mentioned the importance of not being too restrictive of the development of new movement solutions. Could you share any examples from your own practice where you’ve aimed to create an environment that encourages variability and exploration? “So, for example, when you’re trying to do a lunge exercise – and with ACL injuries, there’s a very common concern about knee valgus as a faulty movement pattern. Now, if it’s really faulty or not can be discussed, but I don’t think that’s within the scope of our conversation. But if you want to avoid that exposure, instead of telling them ‘Don’t bring your knee inward’, you can constrain the environment using an external reference – for example a stick, a cone, whatever – to make sure that the patient travels the knee towards this object. That would be one example. With ACL injuries, you also have the example of landing tasks. […] When patients start practicing landing, they tend to avoid knee flexion […] So in that case, you might say ‘I want you to land to the level of a certain object’, to make sure they go deeper into flexion.” Once I heard you say, ‘I don’t treat a knee injury, I treat a patient with a knee injury’. Could you explain what you meant by that? “When you only read research, it can sometimes create the illusion that everything is black and white, that things are very straightforward […]. For example, with ACL patients, you often see protocols that say you should do certain exercises at certain stages. It’s very common. So, you can build up expectations ‘At three months, the patient needs to be running’ or ‘At four weeks, they need to be without crutches.’ But then, in the real world, things aren’t this clear, because the injury and the impact that an injury can have on an individual are two completely different things. That will affect the rehabilitation process completely. So, it’s important not to forget that we need to integrate what research tells us with the reality of the person in front of us. They might be stressed, anxious, avoiding movement, catastrophizing the injury, or they might be confident and ready to move forward. […] The fact that you have different people who react differently to injury […] is going to have a huge influence on how we work and how the person responds to what we do. […] I probably heard that sentence somewhere else, but I think that’s so important, because the person always comes first. They dictate where the treatment goes […]”. So, you mentioned that phrase to support a patient-centred approach. When I first heard it, I understood it as the need to develop exercises that not only target the injured knee – the damaged structure – but also consider all the interactions that have been altered throughout the body system. […] Have you ever come across Bernstein’s work on motor control? “A little, a very little”. Well, our body is a complex system made up of various components, such as muscles and joints, which allow for multiple degrees of freedom for movement. And Bernstein showed that, to achieve the same task, we can use different combinations of degrees of freedom, which result in a wide range of possible movement solutions. So, he raised the question of how we can make such a complex system controllable. Well, the idea is that we develop couplings between these degrees of freedom as we learn how to move. To what extent would you use this perspective to guide your clinical practice? “I’m not extremely familiar with Bernstein, I don’t want to mischaracterize the concepts or anything. […] But the way I think about it is more in terms of having too many options, and then turning that into something more efficient […] But we deal with the opposite […] after an injury, people tend to lose those options […], so we’re not coming from a place with a lot of abundance in terms of strategies, we’re coming from someone who has very little options to produce a certain movement or achieve a certain task. So, I would find it quite challenging to think in that way when it comes to a person with an injury […] it is quite well established that people lose movement options and movement variability… So, your role would rather be to encourage this variability again or to… “Yes, exactly. Yes, that’s exactly what I mean”. And how would you do that, practically? “[…] For example, a judo athlete can develop an episode of low back pain. When you’re in pain, your body becomes stiff and protective towards some movements. So, the range of movement strategies that the athlete uses to do certain tasks is reduced; they cannot move properly because they are in pain. […] You can use many mobility exercises, for example, as an approach to make sure they explore those degrees of freedom in order to develop these movement strategies once again. […] If they’re in pain, they’re not going to move; if your ankle hurts too much, you’re not going to start jumping! So, controlling pain is essential to building some motor abilities. […] To be honest, just exposing the person to the task, I think, that’s the best way to help develop those strategies. We sometimes overthink, but the body will self-organize and get that complexity back without needing too much information from the therapist’s side. That’s my opinion, and that’s how I try to deal with it. So, it’d be too corrective to say ‘Try to be like this, don’t try to be like that’; once again, just let the person go into the field. And then if you need to constrain the environment in ways that promote more variability, I mean, that’s fine… but give the person some foundational levels of physical capacity, control pain, then let them go.” Could you please give me your own definition of rehabilitation? “Oh !!… It’s the process of bringing a person back to the levels of function and quality of life, to the level they had before the traumatic event injury; and when that is not possible, because of chronical conditions like fibromyalgia, rehabilitation becomes the process of helping the patient live with disability and manage disability the best they can. […] So, the concept of rehabilitation can change for each condition, specifically.” Extracts from the interview with Physiotherapist B: Let’s say you give a certain exercise to a patient, but as soon as they start to move, you feel that something in the way they’re doing it could be unhealthy – maybe it could present a risk of reinjury. How would you respond in that situation? “As I shared with you before, pain is always the clinical symptom that makes me think ‘Okay, I’m going too fast’ or ‘I’m going in the wrong way; we need to try another thing. Maybe we need to reverse the loads… yes, it’s more about that!’” So – correct me if I’m wrong – you’re more focused on helping the patient control their pain, rather than making them achieve an ideal movement pattern? “That’s it, that’s it! Because if an athlete has no pain, they can do everything. Like kids. Make them play, play, play… and they’re going to learn. So, they’re quite free in a way? “Yes, yes. But I always respect the principles of strength training and overload. I need to be present, but we can play through a lot of exercises.” What kind of exercises? Would you design exercises that specifically target the injured structure, or rather exercises that involve different body components to build up interactions between them? “[…] I mean, you just go with strength training. You can’t go wrong getting strong! […] Strength, I think it’s the most important thing to prevent injuries”. How about after getting strong again – how would you guide the patient relearn how to move? “Play! It’s always about having fun. […] Sometimes I play football with them, sometimes we hit some volantes (shuttlecocks). […] My role in clinic isn’t so much about performance or improving physical qualities; it’s more about resolving a problem, a symptom – usually pain, or instability. And after that, sharing the information with their strength and conditioning coach. And that’s a difficult question”. Could you please give me your own definition of rehabilitation? “Rehabilitation could be… the process of restoring the ability to function.” |
However, alongside the clearly and consistently established patient-centred approach, rehabilitation practice was not firmly rooted in any single, defined theoretical framework. For instance, both the constraints-led approach (CLA) – which draws from a systems perspective (please refer to Subsection 1.2.2. for more details) – and explicit instructions regarding segment alignment were interchangeably used to influence patient behaviour.
CLA was employed through various methods. The use of equipment to define task goals and constrain patient behaviour was notably advocated for ACL rehabilitation (Table 3, e.g., Physiotherapist A’s response to the first question). Analogies and metaphors were also used as constraints to encourage specific movement solutions. For example, a physiotherapist aimed to adjust Patient 15’s upper limb movement by introducing the following metaphorical constraint during a traction exercise: “Do it again, but this time as if someone behind you should be able to read the time on your watch”. Also, physiotherapists relied on environmental constraints to guide the discovery of new movement solutions. For instance, to reduce the undesired trunk rotations exhibited by Patient 10 during a knee flexion-extension exercise, the physiotherapist repositioned the slopped surface the patient stood on against a wall, then specified: “Do the same exercise, while keeping your hands in touch with the wall!”. Finally, the use of aquatic exercises for Patient 9 – aimed at practicing movements not yet achievable on land – may recall the experimental study conducted by Thelen and colleagues, in which submerging infants’ legs in water was used to reduce the effects of leg mass and facilitate stepping movements (88). The physiotherapist’s additional statement “We can also play around with different levels of water” highlights an approach based on manipulating constraints to enable the patient to explore new movement patterns. In this case, water depth serves as an environmental constraint that interacts with individual constraints – i.e., body mass and strength – by altering their effect on movement through changes in gravitational resistance. This supports the relearning of movement patterns that are either potentially harmful or not yet achievable on land.
On another hand, explicit instructions on how to correctly align body segments during exercise were observed several times with ACL patients. To cite some examples, Patient 12 was asked “not to shift the trunk forward or backward” in a knee flexion-extension exercise with elastic band, and manual adjustments by the physiotherapist were observed twice to correct trunk displacement. Inversely, when the exercise given to Patient 9 focused on trunk rotation while holding weight, the verbal instruction “Do not move your knee” was prescribed to avoid knee rotation. Patient 10 – another ACL patient – also received similar rules on how to correctly position their limbs when performing tasks on various surfaces (e.g., “Press your foot deeper into the BOSU”, “Raise your knee higher when jumping on the trampoline! Stretch and bend!”, “Extend even more your knee”, “Keep your leg higher”). This focus on replicating the proper alignment of body segments to accomplish a task belongs to the traditional cognitive framework of Motor Control. A striking example of this approach was highlighted during a discussion with a physiotherapist regarding certain ACL patients who tended to land excessively forward after jumping. Two methods were proposed to address this issue: 1) providing clearer instructions and 2) adding a mirror to enhance the patient’s body perception. The concept of body perception is crucial to the cognitive, top-down approach because it supports movement control through information processing via internal schemes, mental representations, and sensory feedback.
Overall, rehabilitation practices were influenced by different conceptual frameworks of Motor Control (e.g., traditional cognitive approach vs. ecological dynamics approach), which were sometimes combined to achieve the same clinical goals. For example, while addressing the importance of movement quality in patients, a physiotherapist gave a three-step response to the question “What would you do if a patient did an exercise in a way you would not like to induce?”. The first step was to repeat or reformulate instructions – “do this, don’t do that” – to be certain that the patient understood the exercise. For example, a stand-to-sit exercise could be prescribed with more specific instructions, such as “do it in an upper position without leaning”. As mentioned earlier above, this tendency to provide clearer instructions to correct the patient’s segmental positioning is rooted in the cognitive approach to Motor Control. The physiotherapist then added that this first step might lead to a “weird way of moving without leaning” and “an exaggerated upright posture only after sitting”. In response, the physiotherapist could propose an alternative way of presenting the task by saying: “sit just like if you have a necklace and want everybody around to see it”. This second step is more aligned with a systems approach to Motor Control, using a constraints-led approach (CLA) (i.e., analogical constraints in this case) to encourage healthier movement solutions. Finally, if the patient still does not perform the exercise properly, the third step consists of acknowledging that the patient may not be ready yet to do the task – likely due to insufficient force preparation – and redirecting them to a more appropriate task. This third step reflects a patient-centred approach, which, as explained earlier above, draws on the principles of a systems perspective.
Also, the integration of different conceptual frameworks was sometimes more nuanced. For example, the physiotherapists emphasized the importance on involving the whole body in the rehabilitation process. One physiotherapist working with Patient 9 said, “I like working on both legs during the early stages; we cannot just focus on the operated side.” Similarly, a physiotherapist working with Patient 8 also explained, “When dealing with an ACL injury, it is important to also engage the hip and pelvis in exercises, as they also contribute to postural stability.” This clinical approach reflects a systems perspective to rehabilitation, emphasizing the interconnectedness of body segments in restoring function. However, this can be nuanced by the use of a dynamometer to assess eversion force symmetry (or asymmetry) between the injured and contralateral ankles in Patient 2. Indeed, as previously developed in the first part of the Toolbox (please refer to Subsection 1.1.4.), using limb symmetry indexes as an assessment method can oversimplify the complex alterations following a ligament injury by reducing them to a one-leg problem.
To cite another example illustrating how the connection between theory and practice can be intricate, the clinical goal of restoring 0° knee extension in an ACL patient (e.g., Patient 8) can be interpreted and justified within both cognitive and systems-based frameworks. On the one hand, the emphasis on achieving the “correct 0°-pattern” rather than on achieving a functional task is grounded in a cognitive approach. On the other hand, the physiotherapist further explained that having full range of motion (ROM) supports functionality in everyday life. In this sense, the clinical objective can be interpreted as a way of modifying individual constraints to expand the body’s degrees of freedom, thereby enabling a greater range of movement solutions when facing a motor problem.
Exercises aimed at controlling knee swelling in ACL patients (e.g., Patient 9) can also be interpreted as efforts to enrich their behavioural repertoire with additional movement solutions and, subsequently, restore functionality. Similarly, although Patient 15 presented a prominent acromion bone, the primary focus of their exercises (e.g., rod manipulation) was on improving functional movement rather than simply reducing the bone’s prominence.
In the same vein, strength and pain can also be understood as individual constraints on movement. Physiotherapist A’s interview provided a clear understanding of these factors from a systems perspective (Table 3):
“To be honest, just exposing the person to the task, I think, that’s the best way to help develop those strategies. We sometimes overthink, but the body will self-organize and get that complexity back without needing too much information from the therapist’s side. That’s my opinion, and that’s how I try to deal with it. So, it’d be too corrective to say ‘Try to be like this, don’t try to be like that’; once again, just let the person go into the field. And then if you need to constrain the environment in ways that promote more variability, I mean, that’s fine… but give the person some foundational levels of physical capacity, control pain, then let them go.”
Additionally, a physiotherapist elaborated on the similarities between the objectives of Physical Education and Physical Therapy in helping students or patients with various abilities (re)learn a task. Although the approaches of physical educators and physical therapists can be similar, certain mistakes in rehabilitation are not permitted, as they could increase the risk of reinjury. Within this argument, strength and pain are also viewed as constraints that must be managed when exposing a patient to a task.
Other elements from interviews supported this point (Table 3; e.g., “if your ankle hurts too much, you’re not going to start jumping! So, controlling pain is essential to building some motor abilities”; “You can’t go wrong getting strong!”). In this context, the many repetitive exercises observed in each patient’s rehabilitation programme were designed to “respect the principles of strength training and overload” (Table 3), rather than to implement a cognitive approach to Motor Learning focused on repetition for acquiring and reinforcing new motor skills through memory processes. This distinction in using knowledge from the Physiology and Motor Control fields was clearly expressed (e.g., “Force regain and motor control are two different things”, during a conversation about Patient 9 relearning how to run).
As for pain, it was viewed as a subjective experience (e.g., “You do not treat the body like you fix a car; it is more than replace and go”) that helps guide the rehabilitation process (e.g., “Pain should be assessed during and after an exercise to shape the next exercise”,or Physiotherapist B’s first answer in Table 3:“pain is always the clinical symptom that makes me think ‘Okay, I’m going too fast’ or ‘I’m going in the wrong way; we need to try another thing”). Moreover, pain was considered as a great indicator for RTS (e.g., Physiotherapist B’s second answer in Table 3: “if an athlete has no pain, they can do everything. Like kids. Make them play and they’re going to learn”). To sum up, it seems that clinicians aimed to apply a systems approach byallowing patients to“play”, “go into the field” and “self-organize” (Table 3) during various exercises, while carefullymanaging individual constraints such as strength and pain to ensure both functional and safe movement exploration. This mindset was echoed in Physiotherapist B’s response to the interview question, “How about after getting strong again – how would you guide the patient to relearn how to move?”: “Play! It’s always about having fun.” (Table 3). Finally, both Physiotherapists A and B concluded that restoring function was the core concept of rehabilitation (Table 3), adding that “the best rehabilitation is to keep the patient in touch with their activities, even at early stages”, “because athletes always find out solutions to keep on playing.” During this secondment at R’Equilibri_us clinic, Patient 2 landed a kickflip (i.e., skateboarding trick) upon the request of a physiotherapist, and Patient 3 performed tasks using a metronome similarly to how timing is counted in ballet. In addition, Patient 5 had already returned to Jiu-Jitsu club training but continued to avoid certain movements, which were still being practiced in the clinic under physiotherapist supervision. Last but not least, the main exercises performed by Patient 13 and Patient 14 in the clinic was playing padel under specific rules – for example, using only the ball during the first session, then introducing the racquet in the following sessions with constraints related to backhand and forehand options (Figure 2). Fittingly, one physiotherapist’s mantra captures the spirit of the clinic: “In rehabilitation, it’s important to have fun!”.

Conclusion:
Building the bridge between research and practice
While the first and second parts of this Toolbox addressed to the extent to which sports injuries were approached from a systems perspective in research and clinic, respectively, this conclusion section aims to build the bridge between these two components. This section hence outlines both current efforts and future directions to establish an efficient dialogue between research and clinical practice.
Efforts to translate knowledge of Motor Control into rehabilitation practice have long been underway from the research side. Over thirty years ago, John P. Scholz – who made significant contributions to the field of Motor Control from a systems perspective – was already working to translate dynamical systems principles into clinical practice by developing a step-by-step methodology that therapists could use to assess and guide meaningful movement change in rehabilitation (23). Moreover, he stressed the importance of maintaining a strong connection between theory and experiment, ensuring that scientific foundations could meaningfully inform clinical application. As another example of translation into practice, two decades later, R.T. Harbourne and N. Stergiou developed a practical therapy guide that used concrete clinical scenarios to demonstrate how insights from complex nonlinear systems and movement variability could inform and advance rehabilitation practice (51).
Clinicians also play a key role by informing rehabilitation strategies with evidence-based practice and engaging in scientific meetings and professional platforms to foster dialogue and innovation. At the R’Equilibri_us clinic, physiotherapists have expressed a high interest in the scientific literature, with particular emphasis on strength training principles, while interest in motor control concepts appears to be emerging or less central. Moreover, their participation to surveys that serve as a channel between clinical experience and academia underscores an active willingness to strengthen the dialogue between researchers and therapists. Furthermore, the R’Equilibri_us physiotherapists played a key role in closing the translation loop within the researcher-clinician-patient system by sharing with patients a decision aid website for ACL injury treatment options (https://www.aclinjurytreatment.com/), developed by university professor S. Filbay in collaboration with clinicians to ensure it was accessible and patient-friendly.
Finally, this Toolbox itself reflects an effort by the REPAIRS European Training Network to strengthen the connection between research and clinical practice. During this secondment, on-field observations, discussions and interactions between the ESR12 research student, R’Equilibri_us physiotherapists and patients with various sports injuries contributed to promote the necessary dialogue between all rehabilitation actors. In addition, the ball-and-board task developed in the context of ESR12’s research project to study the potential benefits of joint action in the relearning of postural stability (87,89) was tested at the R’Equilibri_us clinic, providing concrete feedback from both an ACL patient (i.e., Patient 7) and a healthcare professional (Figure 3). This joint-action game consists of jointly manipulating a board to guide a rolling ball along a circular target path, all while standing on an unstable surface (BOSU). Patient 7 reported that the game became physically demanding toward the end of the 60-second trial. The physiotherapist highlighted the game’s relevance for Patient 7, noting that early-stage ACL rehabilitation should emphasize building quadriceps and hamstring strength, as well as improving balance control. Regarding joint-action specificity, he recommended improving the game’s clinical applicability, in addition to further validating it with patients. In its current form, this joint-action game makes clinical assessment challenging, as the physiotherapist must focus on both balance and ball control, which limits their ability to observe the patient’s movements.
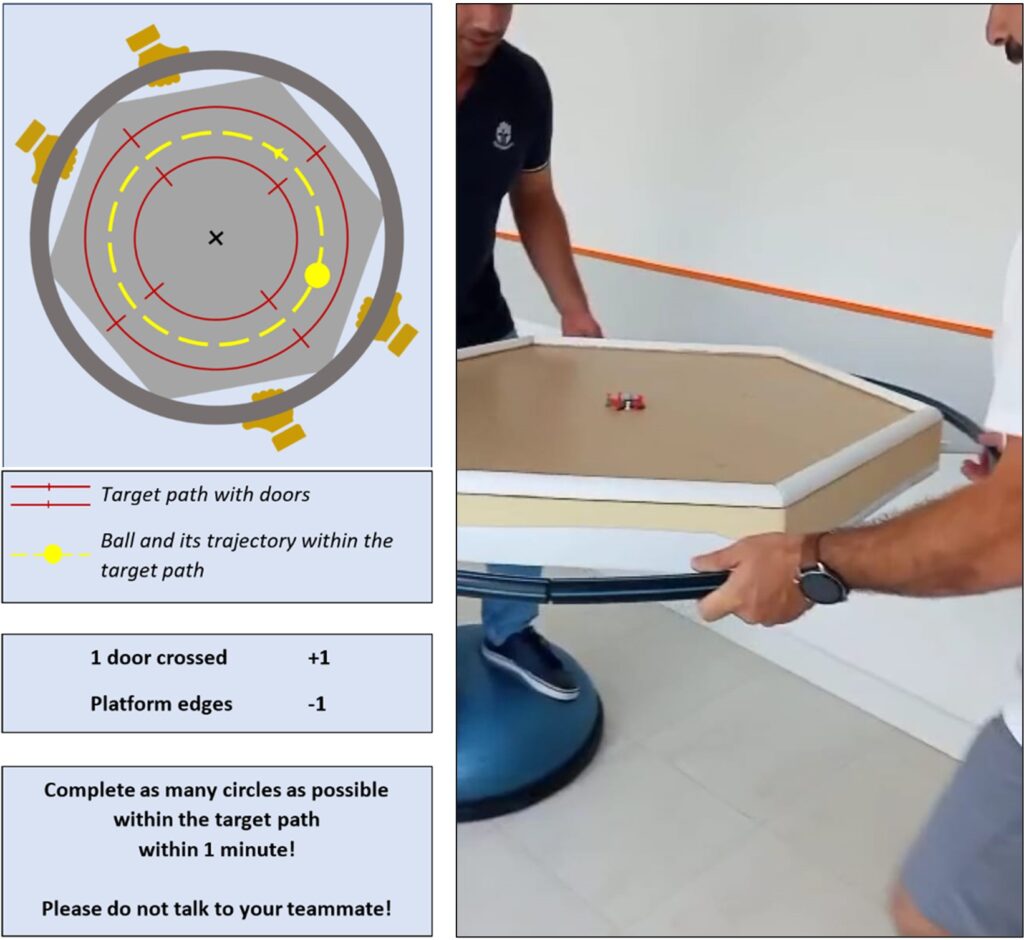
Beyond these Toolbox and secondment, the REPAIRS European Training Network have encouraged diverse interactions between researchers and healthcare partners, including the R’Equilibri_us physiotherapy clinic (Portugal), the MEDIAN rehabilitation centre (Germany), the Revalidatie Friesland rehabilitation centre (Netherlands), the ONCE Fundation (Spain), which promotes social and professional inclusion of people with disabilities (and particularly visual impairments), the Bruno Kessler Fondazione (Italy), specialized in developing advanced healthcare technologies, and the APAR association (France), dedicated to supporting individuals with autism and their families.
Despite decades of intensified efforts to bridge the gap between research and clinical practice, substantial challenges persist and remain to be addressed. For example, the REPAIRS research initiative was built on six pillars, each connecting two of the four following levels of analysis: neural, movement, agent-environment and agent-agent. Additionally, a seventh pillar addresses research questions related to translation into clinical, technological and philosophical areas. Although the interdisciplinary, intersectoral, and international scope of the REPAIRS network offers a comprehensive perspective on motor control applications in rehabilitation, the programme did not account for complex and multifactorial processes such as pain and fear of reinjury, which should be regarded as critical constraints in shaping the emergent behaviours of individuals with motor disorders.
A systems-based understanding of pain and fear of (re)injury has only recently emerged in the scientific literature. Using a systems perspective, Vaz and colleagues defined chronic musculoskeletal pain as “an embodied, embedded, and enactive process of experiencing a closed-off field of affordances (i.e., shutting down of action possibilities)” (p. 10) (26). Such an ecological conception of pain avoids stigmatizing patients by rejecting dualistic separations between agent and environment, or body and mind. Rather, it highlights that musculoskeletal pain is experienced through the patient’s body (i.e., embodied), situated within a physical and social environment (i.e., embedded), and arises from the patient’s active interaction with this environment (i.e., enactive). Furthermore, this systems-based conceptualization of pain informs the development of clinical practices that are aligned with its principles. Whereas interventions aimed at reproducing “correct” movement patterns may inadvertently reinforce fear-avoidance behaviours in patients, an ecological-guided approach that opens up their field of affordances promotes the reshaping of perceptions through movement exploration and gradual exposure to feared activities.
In practice, this expansion of action capabilities in feared situations can be fostered by creating a meta-stable performance environment – one that enables patients to transition from their initial, stable, perceived-as-safe behaviours towards the exploration of new, perceived-as-unsafe movement patterns (90). To put it differently, movement exploration in the context of fear of re-injury can be encouraged by a constrained environment that offers new action possibilities, while also allowing patients to exploit fall-back solutions from their pre-existing behavioural repertoire. The application of an ecological dynamics approach into clinics can thus be designed to recognize pain and fear as existing constraints on patients’ behaviours during the re-learning of perception-action couplings.
While efforts to bridge research and clinical practice have grown over the past decades, they may still represent only the early stages of a deeper, more cohesive connection. The present Toolbox was designed to support this advancement, emphasizing the critical importance of communication between researchers and therapists. In both areas, the patient’s feelings and needs must be prioritized to ultimately enhance their quality of life. Looking ahead, advanced rehabilitation should emerge from exploring the interactions within the patient-clinician-researcher system. Finally, moving beyond traditional cognitive models focused on “having in head”, professionals advancing the rehabilitation field should adopt a systems perspective to Motor Learning grounded in ecological dynamics principles, which support the original etymological spirit of rehabilitation “to have in hand”.
Acknowledgments
We would like to thank all professionals and patients at the clinic R’Equilibri_us for their warm reception and the thoughtful interest they have shown in our research and presence among them.
References
1. Kamm K, Thelen E, Jensen JL. A dynamical systems approach to motor development. Phys Ther. 1990;70(12):763–75.
2. Van Dijk L, Van Der Sluis C, Bongers RM. Reductive and Emergent Views on Motor Learning in Rehabilitation Practice. J Mot Behav. 2017 May 4;49(3):244–54.
3. Schöllhorn WI, Rizzi N, Slapšinskaitė-Dackevičienė A, Leite N. Always Pay Attention to Which Model of Motor Learning You Are Using. Int J Environ Res Public Health. 2022 Jan 9;19(2):711.
4. Schmidt RA. A schema theory of discrete motor skill learning. Psychol Rev. 1975;82(4):225.
5. Gibson JJ. The ecological approach to visual perception. Moughton Mifflin. 1979;
6. Bernstein Ν. The co-ordination and regulation of movements. Oxford Pergamon. 1967;
7. Haken H. Synergetics: An approach to self-organization. Self-Organ Syst Emergence Order. 1987;417–34.
8. Newell KM. Constraints on the development of coordination. Mot Dev Child Asp Coord Control. 1986;
9. Bootsma RJ. Ecological movement principles and how much information matters.
10. Warren WH. The dynamics of perception and action. Psychol Rev. 2006 Apr;113(2):358–89.
11. Chouliaras V, Passler H. The history of the anterior cruciate ligament from Galen to double-bundle ACL reconstruction. Acta Orthop Traum Hell. 2007;12:127–31.
12. Piedade SR, Leite Arruda BP, Antunes de Vasconcelos R, Parker DA, Maffulli N. Rehabilitation And Advances In Surgical Reconstruction For Anterior Cruciate Ligament Insufficiency: What Has Changed Since The 1960s? – State Of The Art. J ISAKOS. 2022 Nov;S2059775422000943.
13. Schindler OS. Surgery for anterior cruciate ligament deficiency: a historical perspective. Knee Surg Sports Traumatol Arthrosc. 2012 Jan;20(1):5–47.
14. Flagg KY, Karavatas SG, Thompson S, Bennett C. Current criteria for return to play after anterior cruciate ligament reconstruction: an evidence-based literature review. Ann Transl Med. 2019 Oct;7(Suppl 7):S252.
15. Gasibat Q, Jahan AM. Pre and post-operative rehabilitation of anterior cruciate ligament reconstruction in young athletes. Int J Orthop Sci. 2017 Jan 1;3(1l):819–28.
16. Kaplan Y, Witvrouw E. When Is It Safe to Return to Sport After ACL Reconstruction? Reviewing the Criteria. Sports Health. 2019 May 28;11(4):301–5.
17. McGrath TM, Waddington G, Scarvell JM, Ball N, Creer R, Woods K, et al. An Ecological Study of Anterior Cruciate Ligament Reconstruction, Part 2: Functional Performance Tests Correlate With Return-to-Sport Outcomes. Orthop J Sports Med. 2017 Feb 1;5(2):232596711668844.
18. Schilaty ND, Nagelli C, Bates NA, Sanders TL, Krych AJ, Stuart MJ, et al. Incidence of Second Anterior Cruciate Ligament Tears and Identification of Associated Risk Factors From 2001 to 2010 Using a Geographic Database. Orthop J Sports Med. 2017 Aug 18;5(8):2325967117724196.
19. Bittencourt NFN, Meeuwisse WH, Mendonça LD, Nettel-Aguirre A, Ocarino JM, Fonseca ST. Complex systems approach for sports injuries: moving from risk factor identification to injury pattern recognition—narrative review and new concept. Br J Sports Med. 2016 Nov;50(21):1309–14.
20. Dischiavi SL, Wright AA, Hegedus EJ, Thornton EP, Bleakley CM. FRAMEWORK FOR OPTIMIZING ACL REHABILITATION UTILIZING A GLOBAL SYSTEMS APPROACH. Int J Sports Phys Ther. 2020 May;15(3):478–85.
21. Quatman CE, Quatman CC, Hewett TE. Prediction and prevention of musculoskeletal injury: a paradigm shift in methodology. Br J Sports Med. 2009 Dec;43(14):1100–7.
22. Lough S. Visuo-motor control following stroke: a motorskills perspective. Annexe Thesis Digit Proj 2016 Block 7. 1984;
23. Scholz JP. Dynamic Pattern Theory—Some Implications for Therapeutics. Phys Ther. 1990 Dec 1;70(12):827–43.
24. Wagenaar RC, van Emmerik RE. Dynamics of movement disorders. Hum Mov Sci. 1996;15(2):161–75.
25. Newell KM, Valvano J. Movement Science: Therapeutic Intervention as a Constraint in Learning and Relearning Movement Skills. Scand J Occup Ther. 1998 Jan;5(2):51–7.
26. Vaz DV, Silva PL, Mancini MC, Carello C, Kinsella-Shaw J. Towards an ecologically grounded functional practice in rehabilitation. Hum Mov Sci. 2017 Apr;52:117–32.
27. Holt KG, Wagenaar RO, Saltzman E. A Dynamic Systems: constraints approach to rehabilitation. Braz J Phys Ther. 2010 Dec;14(6):446–63.
28. Eagle SR, Nindl BC, Johnson CD, Kontos AP, Connaboy C. Does Concussion Affect Perception–Action Coupling Behavior? Action Boundary Perception as a Biomarker for Concussion. Clin J Sport Med. 2021 May;31(3):273–80.
29. Eagle SR, Kontos AP, Pepping GJ, Johnson CD, Sinnott A, LaGoy A, et al. Increased Risk of Musculoskeletal Injury Following Sport-Related Concussion: A Perception–Action Coupling Approach. Sports Med. 2020 Jan;50(1):15–23.
30. Watson G, Brault S, Kulpa R, Bideau B, Butterfield J, Craig C. Judging the ‘passability’ of dynamic gaps in a virtual rugby environment. Hum Mov Sci. 2011 Oct;30(5):942–56.
31. Haken H, Kelso JAS, Bunz H. A theoretical model of phase transitions in human hand movements. Biol Cybern. 1985 Feb;51(5):347–56.
32. Kelso JAS. The Haken–Kelso–Bunz (HKB) model: from matter to movement to mind. Biol Cybern. 2021 Aug;115(4):305–22.
33. Pol R, Hristovski R, Medina D, Balague N. From microscopic to macroscopic sports injuries. Applying the complex dynamic systems approach to sports medicine: a narrative review. Br J Sports Med. 2019 Oct;53(19):1214–20.
34. Fonseca ST, Souza TR, Verhagen E, Van Emmerik R, Bittencourt NFN, Mendonça LDM, et al. Sports Injury Forecasting and Complexity: A Synergetic Approach. Sports Med. 2020 Oct;50(10):1757–70.
35. Seay JF, Van Emmerik REA, Hamill J. Low back pain status affects pelvis-trunk coordination and variability during walking and running. Clin Biomech. 2011 Jul;26(6):572–8.
36. Hamill J, Van Emmerik REA, Heiderscheit BC, Li L. A dynamical systems approach to lower extremity running injuries. Clin Biomech. 1999 Jun;14(5):297–308.
37. Kurz MJ, Stergiou N, Buzzi UH, Georgoulis AD. The effect of anterior cruciate ligament recontruction on lower extremity relative phase dynamics during walking and running. Knee Surg Sports Traumatol Arthrosc. 2005 Mar;13(2):107–15.
38. Kiefer AW, Ford KR, Paterno MV, Schmitt LC, Myer GD, Riley MA, et al. Inter-segmental Postural Coordination Measures Differentiate Athletes with ACL Reconstruction from Uninjured Athletes. Gait Posture. 2013 Feb;37(2):149–53.
39. Nematollahi M, Razeghi M, Mehdizadeh S, Tabatabaee H, Piroozi S, Rojhani Shirazi Z, et al. Inter-Segmental Coordination Pattern in Patients with Anterior Cruciate Ligament Deficiency during a Single-Step Descent. PLoS ONE. 2016 Feb 22;11(2):e0149837.
40. Blache Y, Pairot De Fontenay B, Argaud S, Monteil K. Asymmetry of Inter-joint Coordination during Single Leg Jump after Anterior Cruciate Ligament Reconstruction. Int J Sports Med. 2016 Dec 16;38(02):159–67.
41. Park S, Yoon S. Quantifying Coordination and Variability in the Lower Extremities after Anterior Cruciate Ligament Reconstruction. Sensors. 2021 Jan 19;21(2):652.
42. Davids K, Glazier P, Ara??jo D, Bartlett R. Movement Systems as Dynamical Systems: The Functional Role of Variability and its Implications for Sports Medicine. Sports Med. 2003;33(4):245–60.
43. St-Onge N, Duval N, Yahia L, Feldman AG. Interjoint coordination in lower limbs in patients with a rupture of the anterior cruciate ligament of the knee joint. Knee Surg Sports Traumatol Arthrosc. 2004 May 1;12(3):203–16.
44. Smeets A, Verheul J, Vanrenterghem J, Staes F, Vandenneucker H, Claes S, et al. Single-Joint and Whole-Body Movement Changes in Anterior Cruciate Ligament Athletes Returning to Sport. Med Sci Sports Exerc. 2020 Aug;52(8):1658–67.
45. Goldberger AL, West BJ, Bhargava V. Nonlinear mechanisms in physiology and pathophysiology Toward a dynamical theory of health and disease. 1985;
46. Goldberger AL, West BJ. Chaos and Order in the Human Body. CHANCE. 1992 Jan;5(1–2):47–55.
47. Goldberger AL. Non-linear dynamics for clinicians: chaos theory, fractals, and complexity at the bedside. The Lancet. 1996 May;347(9011):1312–4.
48. Lipsitz LA, Goldberger AL. Loss of “Complexity” and Aging: Potential Applications of Fractals and Chaos Theory to Senescence. JAMA. 1992 Apr 1;267(13):1806.
49. Vaillancourt DE, Newell KM. Changing complexity in human behavior and physiology through aging and disease. Neurobiol Aging. 2002 Jan;23(1):1–11.
50. Stergiou N, Decker LM. Human Movement Variability, Nonlinear Dynamics, and Pathology: Is There A Connection? Hum Mov Sci. 2011 Oct;30(5):869–88.
51. Harbourne RT, Stergiou N. Movement Variability and the Use of Nonlinear Tools: Principles to Guide Physical Therapist Practice. Phys Ther. 2009 Mar 1;89(3):267–82.
52. Birch CE, Mensch KS, DeSarno MJ, Beynnon BD, Tourville TW. Subchondral Trabecular Bone Integrity Changes Following ACL Injury and Reconstruction: A Cohort Study with a Nested, Matched Case-Control Analysis. Osteoarthritis Cartilage. 2018 Jun;26(6):762–9.
53. Decker LM, Moraiti C, Stergiou N, Georgoulis AD. New insights into anterior cruciate ligament deficiency and reconstruction through the assessment of knee kinematic variability in terms of nonlinear dynamics. Knee Surg Sports Traumatol Arthrosc. 2011 Oct;19(10):1620–33.
54. Negahban H, Sanjari MA, Karimi M, Parnianpour M. Complexity and variability of the center of pressure time series during quiet standing in patients with knee osteoarthritis. Clin Biomech. 2016 Feb;32:280–5.
55. Georgoulis AD, Moraiti C, Ristanis S, Stergiou N. A Novel Approach to Measure Variability in the Anterior Cruciate Ligament Deficient Knee During Walking: The Use of the Approximate Entropy in Orthopaedics. J Clin Monit Comput. 2006 Apr 10;20(1):11–8.
56. Moraiti CO, Stergiou N, Ristanis S, Vasiliadis HS, Patras K, Lee C, et al. The Effect of Anterior Cruciate Ligament Reconstruction on Stride-to-Stride Variability. Arthrosc J Arthrosc Relat Surg. 2009 Jul;25(7):742–9.
57. De Oliveira EA, Andrade AO, Vieira MF. Linear and nonlinear measures of gait variability after anterior cruciate ligament reconstruction. J Electromyogr Kinesiol. 2019 Jun;46:21–7.
58. Cavanaugh J, Guskiewicz K, Giuliani C, Marshall S, Mercer V, Stergiou N. Detecting altered postural control after cerebral concussion in athletes with normal postural stability. Br J Sports Med. 2005 Nov;39(11):805–11.
59. Cavanaugh JT, Guskiewicz KM, Stergiou N. A Nonlinear Dynamic Approach for Evaluating Postural Control: New Directions for the Management of Sport-Related Cerebral Concussion. Sports Med. 2005;35(11):935–50.
60. Cavanaugh JT, Mercer VS, Stergiou N. Approximate entropy detects the effect of a secondary cognitive task on postural control in healthy young adults: a methodological report. J NeuroEngineering Rehabil. 2007 Oct 30;4:42.
61. Purkayastha S, Adair H, Woodruff A, Ryan LJ, Williams B, James E, et al. Balance Testing Following Concussion: Postural Sway versus Complexity Index. PM&R. 2019 Nov;11(11):1184–92.
62. Philippe P, Mansi O. Nonlinearity in the Epidemiology of Complex Health and Disease Processes.
63. Bolt R, Heuvelmans P, Benjaminse A, Robinson MA, Gokeler A. An ecological dynamics approach to ACL injury risk research: a current opinion. Sports Biomech. 2021 Aug 10;1–14.
64. Yung KK, Ardern CL, Serpiello FR, Robertson S. Characteristics of Complex Systems in Sports Injury Rehabilitation: Examples and Implications for Practice. Sports Med – Open. 2022 Feb 22;8:24.
65. Larson D, Vu V, Ness BM, Wellsandt E, Morrison S. A Multi-Systems Approach to Human Movement after ACL Reconstruction: The Musculoskeletal System. Int J Sports Phys Ther. 2021;17(1):27–46.
66. Wellsandt E, Failla MJ, Snyder-Mackler L. Limb Symmetry Indexes Can Overestimate Knee Function After Anterior Cruciate Ligament Injury. J Orthop Sports Phys Ther. 2017 May;47(5):334–8.
67. Benjaminse A, Holden S, Myer GD. ACL rupture is a single leg injury but a double leg problem: too much focus on ‘symmetry’ alone and that’s not enough! Br J Sports Med. 2018 Aug;52(16):1029–30.
68. Leventer L, Dicks M, Duarte R, Davids K, Araújo D. Emergence of Contact Injuries in Invasion Team Sports: An Ecological Dynamics Rationale. Sports Med. 2015 Feb;45(2):153–9.
69. Passos P, Milho J, Fonseca S, Borges J, Araújo D, Davids K. Interpersonal Distance Regulates Functional Grouping Tendencies of Agents in Team Sports. J Mot Behav. 2011 Apr 3;43(2):155–63.
70. Hristovski R, Davids K, Araújo D. INFORMATION FOR REGULATING ACTION IN SPORT: METASTABILITY AND EMERGENCE OF TACTICAL SOLUTIONS UNDER ECOLOGICAL CONSTRAINTS.
71. Stone JA, Strafford BW, North JS, Toner C, Davids K. Effectiveness and efficiency of virtual reality designs to enhance athlete development: an ecological dynamics perspective. Dicks M, O’Halloran J, Navarro M, editors. Mov Sport Sci – Sci Mot. 2018;(102):51–60.
72. Levin MF, Demers M. Motor learning in neurological rehabilitation. Disabil Rehabil. 2021 Nov 20;43(24):3445–53.
73. Davis WE, Burton AW. Ecological Task Analysis: Translating Movement Behavior Theory into Practice. Adapt Phys Act Q. 1991 Apr;8(2):154–77.
74. Burton AW, Davis WE. Ecological task analysis utilizing intrinsic measures in research and practice. Hum Mov Sci. 1996 Apr;15(2):285–314.
75. Orangi B Mohammadi, Yaali R, Bahram A, Aghdasi MT, Van Der Kamp J, Vanrenterghem J, et al. Motor learning methods that induce high practice variability reduce kinematic and kinetic risk factors of non-contact ACL injury. Hum Mov Sci. 2021 Aug;78:102805.
76. Orangi B Mohammadi, Dehghani M, Jones PA. Manipulation of task constraints is the most effective motor learning method for reducing risk factors for ACL injury during side-step cutting in both male and female athletes. Res Sports Med Print. 2024;32(4):631–47.
77. Schöllhorn W, Beckmann H, Davids K. Exploiting system fluctuations. Differential training in physical prevention and rehabilitation programs for health and exercise. Medicina (Mex). 2010 Jun 12;46(6):365.
78. I. Schollhorn W. The Nonlinear Nature of Learning – A Differential Learning Approach. Open Sports Sci J. 2012 Sep 13;5(1):100–12.
79. Ghanati HA, Letafatkar A, Shojaedin S, Hadadnezhad M, Schöllhorn WI. Comparing the Effects of Differential Learning, Self-Controlled Feedback, and External Focus of Attention Training on Biomechanical Risk Factors of Anterior Cruciate Ligament (ACL) in Athletes: A Randomized Controlled Trial. Int J Environ Res Public Health. 2022 Aug 15;19(16):10052.
80. Wayne PM, Manor B, Novak V, Costa MD, Hausdorff JM, Goldberger AL, et al. A systems biology approach to studying Tai Chi, physiological complexity and healthy aging: Design and rationale of a pragmatic randomized controlled trial. Contemp Clin Trials. 2013 Jan;34(1):21–34.
81. Wayne PM, Gow BJ, Costa MD, Peng CK, Lipsitz LA, Hausdorff JM, et al. Complexity-Based Measures Inform Effects of Tai Chi Training on Standing Postural Control: Cross-Sectional and Randomized Trial Studies. PLoS ONE. 2014 Dec 10;9(12):e114731.
82. Gokeler A, Neuhaus D, Benjaminse A, Grooms DR, Baumeister J. Principles of Motor Learning to Support Neuroplasticity After ACL Injury: Implications for Optimizing Performance and Reducing Risk of Second ACL Injury. Sports Med Auckl Nz. 2019;49(6):853–65.
83. West BJ, Geneston EL, Grigolini P. Maximizing information exchange between complex networks. Phys Rep. 2008 Oct;468(1–3):1–99.
84. Almurad ZMH, Roume C, Blain H, Delignières D. Complexity Matching: Restoring the Complexity of Locomotion in Older People Through Arm-in-Arm Walking. Front Physiol. 2018 Dec 4;9:1766.
85. Ezzina S, Roume C, Pla S, Blain H, Delignières D. Restoring Walking Complexity in Older Adults Through Arm-in-Arm Walking: Were Almurad et al.’s (2018) Results an Artifact? Motor Control. 2021 Jul 1;25(3):475–90.
86. Riley MA, Richardson MJ, Shockley K, Ramenzoni VC. Interpersonal Synergies. Front Psychol [Internet]. 2011 [cited 2021 Jan 11];2. Available from: http://journal.frontiersin.org/article/10.3389/fpsyg.2011.00038/abstract
87. Cheillan A, Milho J, Passos P. Inter-limb and inter-agent coordination in an original joint-action game: exploring novel approaches for clinical practice. Front Psychol. 2025 Mar 24;16:1514957.
88. Thelen E, Fisher DM, Ridley-Johnson R. The relationship between physical growth and a newborn reflex. Infant Behav Dev. 1984;7(4):479–93.
89. Cheillan A, Milho J, Passos P. Changes in postural stability induced by a ball-and-board game designed from a systems perspective. BMC Sports Sci Med Rehabil. 2025 May 14;17(1):123.
90. Seifert L, Hacques G, Komar J. The Ecological Dynamics Framework: An Innovative Approach to Performance in Extreme Environments: A Narrative Review. Int J Environ Res Public Health. 2022 Feb 27;19(5):2753.